Bowel Disease & Treatments
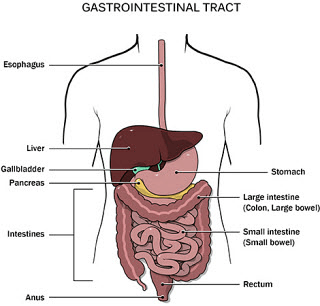
Bowel Anatomy
The bowel is found at the lower part of the digestive system and is at the lower part of the passage along which food passes through the body from mouth to anus during digestion.
The bowel is part of the alimentary canal below the stomach and it is a hollow tube.
The digestive system processes all the food we eat and breaks it down into nutrients for the body.
It also gets rid of any solid waste matter from the body in the form of faeces or stools.
The bowel is divided into two categories:
- The small bowel (or small intestine) is where food is digested and nutrients are absorbed from what we eat.
The large bowel (or colon and rectum) is where water is absorbed from the digested food and forms the stools.
The Large Bowel
The large bowel is about 150cm long and has four sections.
The parts of the colon are the
- Ascending colon – runs up the right side of the abdomen. It is connected to the small intestine by a section of the bowel called the caecum
- Transverse colon – runs across the body from right to left, under the stomach
- Descending colon – runs down the left side of the abdomen
- Sigmoid colon – an 'S-shaped bend that joins the descending colon to the back passage
Non-Cancer Bowel Diseases
Most problems relating to bowel cancer are related to the large bowel. While the small bowel can be obstructed, this is uncommon.
While this page focuses on bowel problems caused by cancer there are other conditions that can affect the bowel and may cause similar symptoms to cancer.
With the right treatment, many of these conditions can be controlled. These include:
- Diverticulitis
- Inflammatory Bowel Disease
- Piles (haemorrhoids) and
- Other infections
Diverticular disease
Diverticulosis consists of small pockets or protrusions of the lining of the large bowel wall through the muscular layer of the bowel and they appear on the outer surface of the large bowel. Diverticulitis occurs when the diverticula are inflamed often in the presence of infection. The most common site of the large bowel that is affected is the sigmoid colon, which is towards the end of the large bowel, just above the rectum.
What causes it?
The condition is associated with a diet that is low in fibre. The condition is very rare in third-world countries where the diet is much higher in fibre than in the standard Western diet.
How common is it?
The condition is rare before the age of 30 but there is an increasing incidence beyond this. In our community, about 60% of people over the age of 50 have diverticulosis. It is a little more common in females than males.
Symptoms of Diverticular disease
The vast majority of people with diverticulosis do not ever develop any symptoms. When inflammation and infection occurs this is called diverticulitis. Symptoms of diverticulitis include
- Abdominal cramping
- Abdominal pain ( usually left sided)
- Altered bowel habit (constipation or sometimes diarrhoea
- Fever
Complications of Diverticular disease
Perforation
If the opening of a diverticulum becomes blocked inflammation may occur. This can be quite localised and this causes fairly severe localised pain, usually in the left lower abdomen, and there may be an associated fever. Subsequently an abscess may form outside the bowel wall and if this becomes large, perforation may occur and this may cause generalised abdominal pain.
Bowel Obstruction
As the result of thickening of the bowel wall and sometimes after scar tissue formation due to repeated episodes of inflammation, the bowel may become so narrow that it blocks the passage of faeces and flatus. Diverticulosis is one of the two most common causes of large bowel obstruction.
Bleeding
A blood vessel in the wall of a diverticulum may become traumatised and bleed. The blood will be either bright or a little dark and this bleeding may be quite significant.
Fistulae
Following a perforation, an abnormal connection with another intra-abdominal organ may occur and this is called a fistula. Organs that may communicate with the large bowel due to diverticulosis include the bladder, the small bowel or the vagina. This may lead to the passage of faeces or flatus in the urine or from the vagina.
Treatment of Diverticular disease
A high fibre diet is usually recommended for patients with diverticulosis. This reduces the pressure within the colon. Foods that are high in fibre include wholemeal and multigrain bread, high fibre cereals, fruit and vegetables. Fibre supplements such as unprocessed bran or psyllium are also useful. Commercially available fibre supplements such as Metamucil or Benefiber may be more palatable.
Treatment sometimes required for acute episodes of diverticulitis include;
- antibiotics;
- bowel rest;
- bland diet; and
- sometimes admission to hospital may be necessary.
Surgery is sometimes necessary for the severe complications of diverticulosis. The large majority of patients with diverticulosis, however, never require surgery.
Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) is a broad term that describes conditions with chronic or recurring immune responses and inflammation of the gastrointestinal tract.
Patients with Inflammatory Bowel Disease have an immune system that mistakes food, bacteria, and other materials in the intestine for foreign substances. This results in their system attacking the cells of the intestines.
The body’s response results in more white blood cells being sent into the lining of the intestines where they produce chronic inflammation.
The two most common inflammatory bowel diseases are
- Ulcerative Colitis
- Crohn’s Disease.
Both illnesses are characterized by an abnormal response to the body’s immune system.
Bowel Cancer
What is Bowel Cancer?
Bowel cancer is the development of malignant cells on the walls of the intestine or rectum.
Most cancers begin as a small growth called a polyp or adenoma and develop into a solid tumour. Research suggests that most bowel (colorectal) cancers can take 5 to 10 years or more to develop.
Bowel cancer typically arise in the colon or the rectum of the large bowel (large intestine). It is for this reason that it is also referred to as Colorectal Cancer.
Bowel cancers start in lining or the innermost tissue layer of the bowel walls.
If left untreated, they may grow into the muscle layers under the lining of the bowel. Then through the bowel wall the malignant cells can then spread into organs that are close to the bowel, such as the bladder, womb, prostate gland or nearby glands (lymph nodes).
Risks of Developing Bowel Cancer
The underlying cause of bowel cancer is not known. It is more common in developed countries and is thought to be due to the food we eat slowing the transit of stools through the bowel.
Bowel Cancer affects more than 4% of Australians with over 12,000 sufferers annually and about 5,000 deaths. Bowel Cancer impacts many people in their older years, especially those over 85.
Lifestyle issues may be important in reducing the risks. Actions to lower risk factors can include:
- regular exercise,
- maintaining ideal weight and
- eating a diet low in fat and high in fibre
- consuming a large amount of tobacco or alcohol
Known factors that will increase your risk are:
- Age - typically over 50
- Having a family history of bowel cancer
- Abnormal growth of cells or polyps on the bowel wall
- Ongoing Inflammatory bowel diseases (Ulcerative Colitis, Crohn’s Disease)
- Genetic conditions like Familial Adenomatous Polyposis – (FAP) or Lynch syndrome
Screening for Bowel Cancer
Despite the persistent incidence of Bowel Cancer in the community, there has been a fall in the overall mortality rate due in part to screening and early intervention and also improved treatments.
Bowel Cancer Screening tests are recommended every 24 months for every Australian over 50.
A chemical test can detect a small amount of blood in the stool and this is called Faecal Occult Blood testing (FOB). This test is performed on samples of stool you collect yourself.
Studies have shown that populations that are screened with a FOB have a lower risk of dying from bowel cancer. Screening programs using FOB are being developed in Australia.
Colonoscopy may also be used as a form of screening and polyp removal. The aim of colonoscopy is to examine your intestine for polyps. Polyps are benign growths occurring on the inner lining of the bowel wall and because they can potentially grow in size and turn into bowel cancer they are removed during the procedure.
Untreated, colon polyp can become cancer.
Those at high risk of colorectal cancer should have a regular screening colonoscopy at least every 3-5 years, with the removal of polyps when they are still small.
Symptoms of Bowel Cancer
Common symptoms of bowel cancer include:
- Change in bowel habits like the onset of diarrhoea or constipation
- Bleeding from the back passage or blood mixed in the stool
- Abdominal pain that persists
- A low blood count or anaemia
Colon cancers rarely cause symptoms until very late.
Rectal cancers may result in bleeding and can be mistaken for haemorrhoids. Rectal cancers may also cause rectal pain on straining or urgency to defecate (tenesmus).
All cancers, if large enough, can cause obstruction, with abdominal bloating and pain very similar to that experienced from constipation.
Tests for Bowel Cancer?
If your doctor suspects you may have bowel cancer, internal examinations of the back passage and special tests will be organised.
Immediate examinations can include:
- A digital examination
- An endoscopic examination using either
- a rigid sigmoidoscopy (up to 20 cms),
- flexible sigmoidoscopy (up to 60 cms)
- colonoscopy (all of the large bowel)
- A biopsy sample of tissue for pathology testing
- CT colonography or X-Ray that outlines the colon
- A CT scan of the abdomen
- An (internal) endorectal ultrasound examination
- MRI scan of the pelvis and rectum
- Occasionally a PET CT is also required to rule out distant spread (metastases).
Stages of Bowel Cancer
Colorectal Cancer is often referred to in stages. These indicate the progression in your body.
- Stage I – tumour is found only in the lining of the bowel
- Stage II – tumour has spread deeper into the layers of the bowel walls
- Stage III – tumour has spread to nearby lymph nodes
- Stage IV – tumour has spread beyond the bowel to other parts of the body, such as the liver or lungs or distant lymph nodes
Almost 50% of bowel cancers disagnosed in Australia are either Stage I or II. Stage IV disease is referred to as metastatic disease.
Due to significant improvements in the treatment of Bowel Cancer over the past decade, excellent results can now be achieved with modern combination treatments.
So despite a poor prognosis with late-stage IV cancer there could still be a role of surgery or combination treatments for late-stage bowel cancer.
Bowel Cancer Survival
The outcome (prognosis) for Bowel Cancer will depend on several factors including:
- The growth pattern of the primary bowel cancer
- The depth cancer has spread through the bowel wall
- The presence of cancer cells in lymph glands and other organs
- A patient's general health and well-being
In patients with cancer confined to the bowel and who undergo an operation, the overall chances of cure are approximately 55%.
About 20% of all patients with bowel cancer present with liver metastases and a further 20% will develop liver metastases at a later stage.
Many patients are suitable for surgery to remove their liver tumours. In patients with isolated liver metastases and who undergo complete resection, approximately 50% will be cured of their disease. This is a dramatic improvement in survival outcomes over the past 20 years compared with the past.
It is a condition that has a good prognosis, with a good chance of cure, if detected in the early stages.
Treatments for Bowel Cancer
The treatments depend on different factors, including the type of bowel cancer you have, its size and whether it has spread (the stage).
Surgery is the main treatment for most people with bowel cancer. You may also have chemotherapy or radiotherapy.
Bowel Cancer Prevention
For patients with rare inherited genetic syndromes:
- Familial Adenomatous Polyposis - FAP
- Lynch syndrome
Further genetic testing and screening for other associated cancers is often indicated
Bowel Cancer Surgery
When bowel cancer has been diagnosed the affected parts of the colon and rectal should be removed quickly.
Bowel surgery is major surgery.
Colorectal cancers, if treated aggressively with surgery frequently do better than other cancers.
The procedures are called:
- colectomy - removal of a portion of colon or bowel resection
- procto-colectomy - removal of the rectum and a portion of the colon
The procedures remove cancer as well as the glands (lymph nodes) that cancer can potentially drain to. The two ends of the healthy bowel are then joined together creating an anastomosis.
In most cases, surgery for colorectal cancer can be performed as a keyhole or laparoscopic procedure. A small incision is then made at the end to deliver the specimen.
Most bowel surgery can usually be performed in an elective manner with the two resected ends of the bowel being connected together as an anastomosis without the need for a diversion to a colostomy bag.
When an emergency bowel surgery is performed due to a blockage a temporary colostomy bag is needed. This could result from the total removal of the anus or rectum.