Haemorrhoids & Rectal Bleeding
Haemorrhoids are a common cause of bleeding from the rectum.
What are Haemorrhoids?
The word “haemorrhoid” describes an enlargement of the normal veins which occur in a patient’s anal canal and the lower rectum.
Normally the vascular structures in the anal canal are cushions that help with stool control.
Haemorrhoids are also referred to as ‘piles’ become pathological when they become wider, swollen, inflamed or engorged with more blood than usual. This can also cause pooling and overlying tissue may then form into one. Haemorrhoids can form either inside or around the end of the anus.
At this point, the condition is technically known as haemorrhoidal disease.
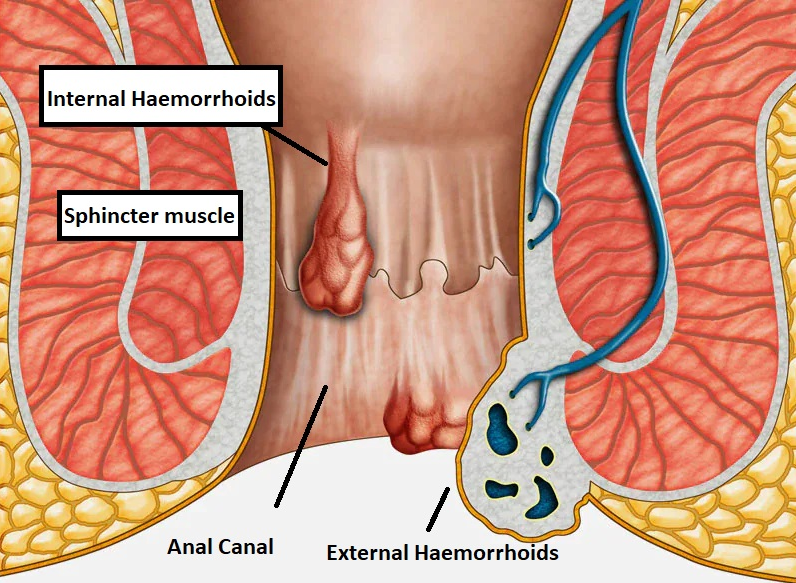
Anatomy of the Anal Canal
At the upper end, the anal canal connects with the rectum (also part of the large intestine). There is a network of small veins (blood vessels) within the lining of the anal canal.
The anal canal is the last part of the large intestine and is about 4 cm long. At the lower end of the anal canal is the opening to the outside (usually referred to as the anus), through which faeces pass.
Causes of Haemorrhoids
Pregnancy is a cause of haemorrhoids. While there are other causes, their link is unclear. Some other possible causes could include:
- Constipation and excess straining on the toilet,
- Diet is pivotal in causing – and preventing haemorrhoids as a lack of dietary fibre vs highly processed foods and inadequate fluid intake are at greater risk
- an inactive lifestyle.
“Weak” veins – leading to haemorrhoids and other varicose veins – may be inherited.
Excess pressure can also be caused by obesity, standing or sitting for long periods, coughing, sneezing, vomiting, and holding your breath while straining to do physical labour.
Types of Haemorrhoids
The signs of haemorrhoids depend on the type present.
- Internal haemorrhoids usually present with painless rectal bleeding, they form above a point 2-3 cm inside the anus in the upper part of the anal canal where no pain nerve fibres exist,
- External haemorrhoids form lower in the anal canal and produce few symptoms where pain nerve fibres exist, and
- Thrombosed Haemorrhoids are caused by clotted veins and can cause significant pain and swelling in the area of the anus.
External haemorrhoids are not always outside of the anal canal (anus) and internal piles can also enlarge and drop-down (prolapse), so that they hang outside of the anus. Patients can also develop internal and external piles at the same time.
Haemorrhoid Classification
Internal piles or Haemorrhoids can be classified into grades 1 to 4 according to their severity and size:
- Grade 1 are small swellings on the inside lining of the anal canal. They cannot be seen or felt from outside the anus. Grade 1 piles are common. In some people, they enlarge further to grade 2 or more.
- Grade 2 is larger. They may be partly pushed out from the anus when you go to the toilet, but quickly spring back inside again.
- Grade 3 protrudes out from the anus when you go to the toilet. You may feel one or more as small, soft lumps that hang from the anus. However, you can push them back inside the anus with a finger.
- Grade 4 permanently protrudes from within the anus, and you cannot push them back inside. They sometimes become quite large.
Frequency of Haemorrhoids
Anyone at any age can be affected by haemorrhoids. However, they are usually more common in elderly people and during pregnancy.
Almost 50% of all patients may experience problems with haemorrhoids at some point in their lives.
Outcomes are usually good.
Haemorrhoid Symptoms
Some people may not even realise they have haemorrhoids, as they do not experience symptoms.
However, when symptoms do occur they may include:
- bleeding after passing a stool (the blood will be bright red)
- Pain can occur when haemorrhoids prolapse (pass into or beyond the anal canal)
- itchiness around your anus (the opening where stools leave the body)
- a lump or a sense on a lump hanging down outside of the anus, which may need to be pushed back in after passing a stool
- a mucus discharge after passing a stool and minor soiling of underwear
- soreness, redness and swelling around your anus.
External haemorrhoids:
- Blood clots may form in the swollen veins causing bleeding, painful swelling or a hard lump.
Patients can incorrectly refer to any symptom occurring around the anal-rectal area as “haemorrhoids” While most cases of fresh rectal bleeding are due to haemorrhoidal bleeding, any person should be assessed and in particular those patients over the age of 50 should be fully investigated with a colonoscopy, to prove that bleeding is not from bowel cancer.
Haemorrhoids Diagnosis
Most important have your colon examined to rule out the possibility of other serious causes of these symptoms.
Your doctor will look at the anal area, perhaps by inserting a lubricated gloved finger and may also decide to use a proctoscope to examine the anorectal region.
If the bleeding has occurred more than once or twice, most patients will require a definitive procedure called either a:
- Colonoscopy: Colonoscopy is a procedure in which a flexible lighted tube is passed through the anus into the rectum and the colon. The colonoscope helps to view the pictures of the inside of the rectum and colon.
- Sigmoidoscopy: This procedure uses a shorter tube called a sigmoidoscope to transmit images of the rectum and the sigmoid colon (the lower portion of the colon).
- These diagnostic procedures can rule out other ailments that can cause anal bleeding, such as
- Anal Fissure,
- Colitis,
- Crohn’s disease.
Because bleeding may also be a sign of large polyps or Colorectal Cancer (or bowel cancer).
Lifestyle Changes as a Treatment for Haemorrhoids
Most cases of haemorrhoids are mild, and the symptoms often disappear on their own after a few days.
Haemorrhoids are not related to abnormal tissue growth and do not increase the chance of other diseases like cancer.
Lifestyle modifications and dietary changes often are helpful in reducing the symptoms of haemorrhoids.
A diet having high fibre content soften the stools and helps to pass them easily thereby avoiding straining. Fruits, vegetables and cereals serve as a good source of dietary fibres.
Fibre supplements such as methylcellulose or stool softeners can be taken. Drinking plenty of water (8-ounce glasses) and adequate exercise helps prevent constipation. Over-the-counter creams and suppositories help relieve the pain and itching.
However, these are short time remedies as long-term use can cause damage to the skin.
Medical Treatments
Conservative Haemorrhoid Management
Treatment of haemorrhoids varies according to the symptoms and degree of prolapse. All patients should
- take steps to avoid straining at stool including:
- increasing fibre and water intake if needed to maintain hydration,
- topical medicines to help with pain, and rest.
- using stool softeners or bulking agents such as Metamucil or Benefibre,
- avoiding constipating medications, and
- responding promptly to the urge to defecate.
- Not sitting on the toilet for long periods of time
As always, if symptoms persist, your doctor should be informed to allow for an informed decision regarding further investigations or treatments.
Interventional Haemorrhoid Treatment
Intervention for haemorrhoids is only required for severe cases or when they cause symptoms that limit normal daily function. Minor procedures can include
- Haemorrhoid Banding uses a tight rubber ligation band around the base of the pile to obstruct the blood supply causing the haemorrhoid to shrink,
- Sclerotherapy: This involves injecting a chemical solution into the blood vessel so that the haemorrhoid shrinks. This Haemorrhoid Injection Therapy (under sedation) uses ‘phenol in oil” to obliterate the blood vessels going to the piles - this can cause a scarring reaction (fibrotic).
Surgical removal becomes necessary when the haemorrhoids are large enough and do not respond to conservative treatment. Haemorrhoid Surgery (under general anaesthetic) to remove or shrink large or external haemorrhoids.
Preventing Recurrence of Haemorrhoids
Once rectal bleeding is diagnosed as haemorrhoids, you can make lifestyle changes to reduce the strain on the blood vessels in and around your anus to prevent recurrent bleeding. These can include:
- gradually increasing the amount of fibre in your diet – good sources of fibre include fruit, vegetables, wholegrain rice, whole wheat pasta and bread, seeds, nuts and oats
- drinking plenty of fluid, particularly water, but avoiding or cutting down on caffeine and alcohol
- not delaying going to the toilet – ignoring the urge to empty your bowels can make your stools harder and drier, which can lead to straining when you do go to the toilet
- avoiding medication that causes constipation – such as painkillers that contain codeine
- losing weight if you are overweight
- exercising regularly – this can help prevent constipation, reduce your blood pressure and help you lose weight
If your stools are lumpy or if you suffer from constipation, you can ask your doctor for specific advice.